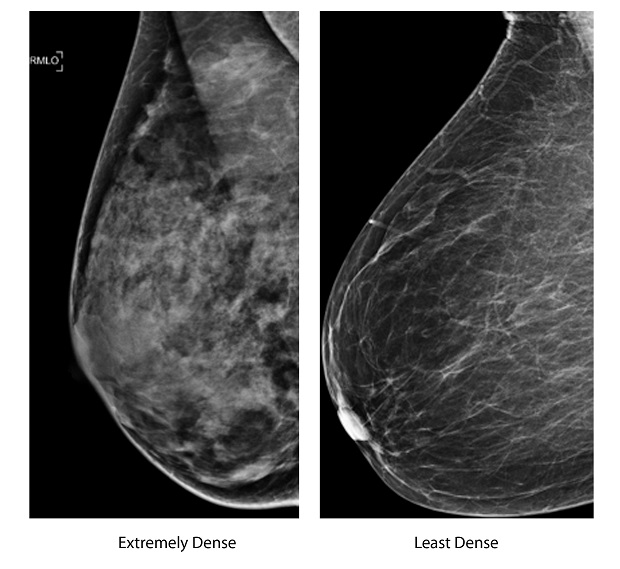
These two undated photos, provided by the American Society of Radiology shows an extremely dense breast, left, and a least dense breast. More women are learning their breasts are so dense that its more difficult for mammograms to spot cancer. But new research suggests automatically giving them an extra test isnt necessarily the solution. AP/American Society of Radiology
WASHINGTON — More women are learning their breasts are so dense that it’s more difficult for mammograms to spot cancer. But new research suggests automatically giving them an extra test isn’t necessarily the solution.
Screening isn’t the only concern. Women whose breast tissue is very dense have a greater risk of developing breast cancer than women whose breasts contain more fatty tissue.
Laws in 19 U.S. states require women to be told if they have dense breasts after a mammogram. Similar legislation has been introduced in Congress.
What’s not clear is what a woman who’s told her breasts are dense should do next, if anything. Some of the laws suggest extra screening may be in order.
Not so fast, a team of scientists reported Monday. They modeled what would happen if women with dense breasts routinely received an ultrasound exam after every mammogram, and calculated such a policy would cost a lot, in extra tests and false alarms, for a small benefit.
For every 10,000 women who got supplemental screening between the ages of 50 and 74, three to four breast cancer deaths would be prevented — but 3,500 cancer-free women would undergo needless biopsies, the study concluded.
“Not everybody with dense breasts is going to get cancer. There are people with dense breasts that are not at high risk,” explained study co-author Dr. Karla Kerlikowske of the University of California, San Francisco, who has long studied density.
Among the questions: How to tell which women really are at high risk, and how to better examine that group.
“We need to investigate alternative screening strategies for women with dense breasts,” added epidemiologist Brian Sprague of the University of Vermont Cancer Center, who led the research published in the journal Annals of Internal Medicine.
Topping that list: Scientists are beginning to study if a newer tool, 3-D mammograms, might get around the density problem by essentially viewing breast tissue from more angles.
Meanwhile, Sprague said his study could help women consider the trade-offs as they decide for themselves whether to pursue an ultrasound.
About 40 percent of women getting mammograms have dense breasts, either fairly widespread density or extremely dense tissue. Fatty tissue appears dark on the breast X-rays. Dense tissue — milk-producing and connective tissue — appears white. So do potentially cancerous spots, meaning they can blend in.
Mammogram reports to doctors have long included information about breast density. But it wasn’t routinely shared with women until some cancer survivors, outraged at not knowing, began spurring state disclosure laws starting in Connecticut in 2009. The advocacy group that started the movement tracks the laws at https://www.areyoudense.org .
What’s a woman to make of the information?
Monday’s study “reaffirms that we don’t know exactly what the right thing to do is when a woman has dense breasts,” said Dr. Otis Brawley, chief medical officer for the American Cancer Society.
Simply finding more tumors won’t necessarily save lives, cautioned Brawley, who worries that “we’re legislating something that we don’t totally understand.”
The American College of Obstetricians and Gynecologists doesn’t recommend routine additional testing in women who have no symptoms or other risk factors.
UCSF’s Kerlikowske said the real issue in deciding whether any woman needs extra screening — from an ultrasound to a more expensive MRI — is her overall risk of breast cancer.
Her team helped create an online risk calculator — https://tools.bcsc-scc.org/BC5yearRisk/ . Plug in age, breast density, if a close relative had breast cancer and a few other details. Putting the risk in perspective, the calculator compares the woman’s chance of developing breast cancer over the next five years with that of an average woman the same age.
But to answer, you have to know just how dense your breasts are.
Radiologists divide density levels into four categories: Almost completely fatty, scattered areas of density, fairly widespread density and the less common extremely dense. There’s no standard way to measure, cautioned the cancer society’s Brawley. And those mailed notifications don’t always give the woman’s category, even though the cancer risk is highest for extremely dense tissue.
Density tends to decrease with age, so a woman’s risk will change over time, Kerlikowske said. It also can reflect some other long-known risk factors, she added. Someone who had children very young probably will have fattier breasts by mammography age than a woman whose first birth was in her 30s.
RELATED STORIES